Dermatophytosis and Dermatomycosis
Discover our DNA extraction for sensitive diagnosis of fungal skin diseases

Disease profile
Dermatophytoses are the most common fungal infections in humans and animals worldwide. They are caused by a specialized group of keratinolytic pathogenic fungi that grow as filaments (hypha). These invade and colonize the stratum corneum of the skin and keratinized tissues, such as smooth skin, skin folds, scalp, and nails or claws. The infection often causes inflammation as the host responds to metabolic byproducts of the dermatophyte invasion. In fact, dermatophytosis represents a sub-category of the clinical representation named dermatomycosis. The latter includes rare infections caused by yeasts such as Candida albicans or mould species, which can affect deeper layers of the skin.
The first recognition that an infection could be caused by a fungus occurred in 1837 when filaments and spores were observed in a chronic infection of the scalp (a condition known today as favus). They were later isolated and attributed to the dermatophyte Trichophyton schoenleinii.
To date, 7 dermatophyte genera comprising more than 40 species have been described. The most frequent species reported from human infections belong to the genera Trichophyton, Microsporum, Nannizzia, and Epidermophyton. According to their natural habitat, dermatophytes are classified into three groups:
- anthropophilic, which only affect humans and cause most of the human cases (ca. 70%)
- zoophilic, with animals as normal hosts but with the ability to infect humans as well
- geophilic, found in soil and only occasionally infecting humans and animals
Both the severity of the dermatomycosis and the aspect of the lesion depend on the associated species, on the site of infection, and on the immunological response of the infected individual. Dermatophyte-caused cases mostly represent superficial infections. Yeast-caused forms of dermatomycoses are sometimes barely noticeable, their clinical manifestations are often associated with erythema, induration, itching, scaling, and even chronic progressive eruptions. These symptoms can last months or years causing considerable discomfort and sometimes even irreversible disfiguration.
Due to the ring shape, snake-like appearance of dermatophyte lesions growing outward on the skin, dermatophytoses are usually named by the word “tinea” (Latin for worm) followed by the Latin name of the infected region.
Perhaps the most known disease caused by a dermatophyte is the athlete’s foot or Tinea pedis. Even in developed countries, it is the most common superficial fungal skin infections, affecting 15% of the global population. Caused by dermatophytes of the genera Trichophyton, Epidermophyton, and Microsporum, it affects the regions between toes and can spread to the sole or even the nails. The condition became more frequent in the 20th century as a result of the greater use of tight-fitting shoes and the infection by walking barefoot in contaminated floors of warm and humid environments such as swimming pools.
Other dermatophytoses include Tinea unguium (ringworm of the nail or onychomycosis), Tinea capitis (ringworm of the scalp), Tinea faciei (facial ringworm), Tinea corporis (ringworm of the body), and Tinea manuum (ringworm of the hands).


Molecular diagnosis
Almost 200 years after the first microscopic description, traditional methods such as direct microscopy of fungal elements in specimens of infected skin, hair or nail, followed by species identification using culture or examination under a Wood’ lamp are still widely used in the diagnosis of dermatomycoses. While these techniques are useful for identification of dermatophytes with their distinguishable morphologic features, they encounter several limitations that can be overcome by molecular techniques. For example, traditional methods require an extended time to diagnosis, cannot always distinguish between morphologically similar species. Molecular methods, however, can accurately and rapidly detect and identify a wide range of clinically relevant fungi - not only after culture but also directly from clinical samples.
The correct identification of the causal agent of a dermatophyte infection to the species level is crucial for various reasons. Apart from allowing for the correct choice and early start of the antifungal treatment (in contrast to over-the-counter medications), it can help determining the origin of infection and managing possible outbreaks. In case of an infection by a zoophilic dermatophyte, the animal, which the fungus is originating from must also be treated.
Molecular diagnostics of dermatophytes mostly involves the use of real-time PCR, designed to detect dermatophyte families or individual species. One of the most advanced approaches combines multiplex PCR with DNA microarray technology. Regardless of the molecular technique of choice, its analytical sensitivity and specificity greatly depends on the quality of the DNA isolated from samples such as skin scrapings, hair or toe-nails. The ideal DNA extraction protocol is not only sensitive but also rapid, simple to conduct, and economical. Its sensitivity greatly relies on the protocol's ability to disrupt the keratin present in the samples enabling access to the actual pathogen.
Our SwiftX technology combines all above features in a eco-friendly, convenient workflow for the extraction of DNA from dermatophytes and other fungal pathogens. The extracted DNA can directly be used in downstream assays such as real-time PCR and microarray-based detection.
Applicable Xpedite Diagnostics products
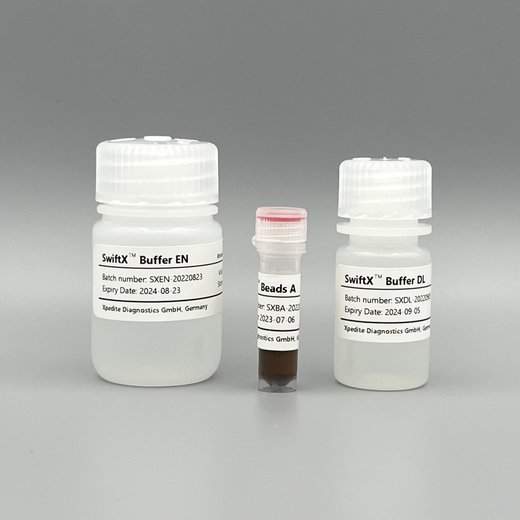
SwiftX™ DNA (25 extractions)
For direct extraction of fungal DNA from dermatophytes, Aspergillus and Candida cells as well as spores. Includes an enzymatic pre-treatment of the samples.
Validated for skin scrapings, hair, and nails.
Go to productUser protocol
Extraction of dermatophyte DNA from skin scrapings, hair, and nails
Helm et al. (2022) Poster at 56th Conference of the German Mycological Society (see below for direct link)
- place a few milligram of sample in a 1.5mL microtube
- add 150μL Buffer DL, 20μL Beads A, 5μL Proteinase K (20mg/mL)
- mix briefly by vortexing
- incubate 10 minutes at 60°C
- incubate 5 minutes at 95°C
- remove microtube from heating block and remove condensate from lid
- place microtube in a magnetic rack and wait 1 minute
- transfer 100μL supernatant to a new microtube